Anesthesia and analgesia for shoulder, upper arm, and clavicle surgeries.
Indications: Anesthesia and analgesia for shoulder, upper arm, and clavicle sugeries
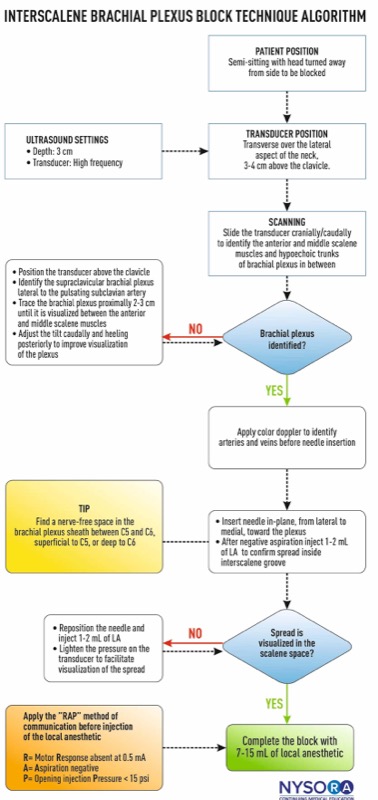
Goal: Local anesthetic spread around superior and middle trunks of the brachial plexus, between the anterior and middle scalene muscles
Transducer: Linear, high frequency
Needle: 23-22 gauge, 5 cm short bevel
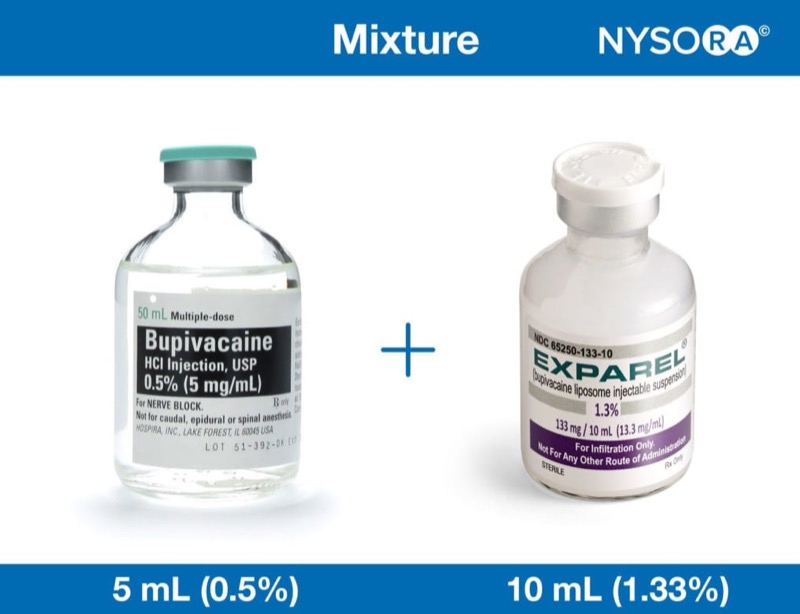
Local anesthetic volume: 7-15 mL
Functional anatomy
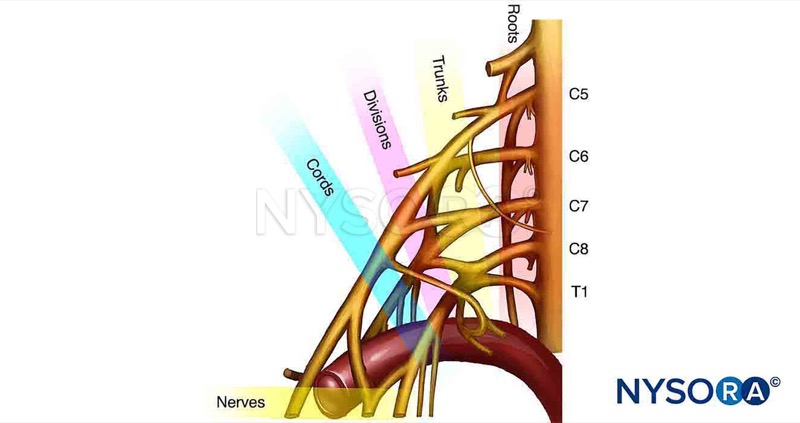
The Brachial Plexus is formed by the ventral rami of the roots C5 to T1 (Fig-1).
These roots join to form the superior (C5, C6), middle (C7), and inferior trunks (C8, T1) above the clavicle.
The trunks then branch into anterior and posterior divisions.
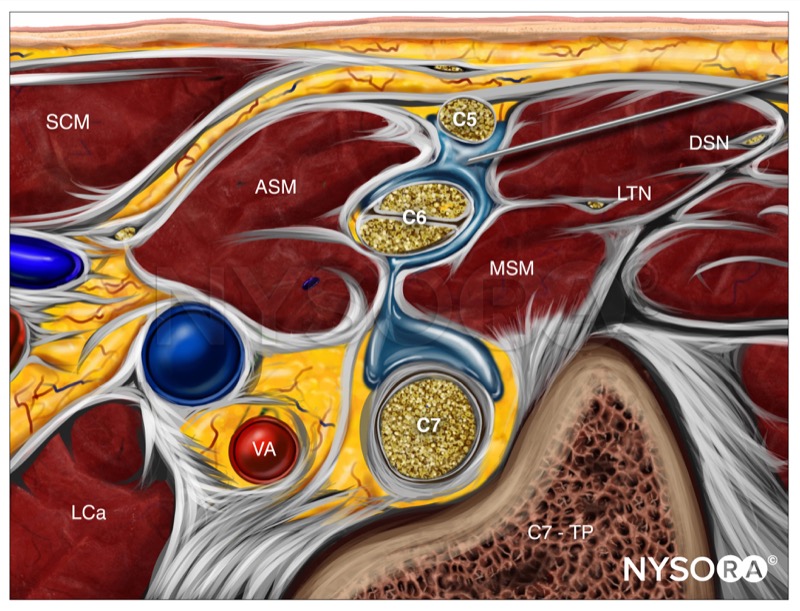
At the interscalene level, the brachial plexus is visualized (Fig-2):
.jpg)
.jpg)
The interscalene brachial plexus block results in anesthesia of the shoulder, upper arm, and lateral two-thirds of the clavicle (Fig-1).
The proximal spread of the local anesthetic outside of the interscalene space commonly blocks the supraclavicular branches of the cervical plexus that supply the skin over the acromion and clavicle.
The inferior trunk (C8-T1) is usually spared with an interscalane approach to the brachial plexus.


When nerve stimulation is used, a number of motor responses of the upper, middle, and inferior trunks of the brachial plexus can be evoked (Fig-2).
Common responses to nerve stimulation in clinical practice are:

 Fig-2. Functional innervation of the upper extremity muscles (myotomes).
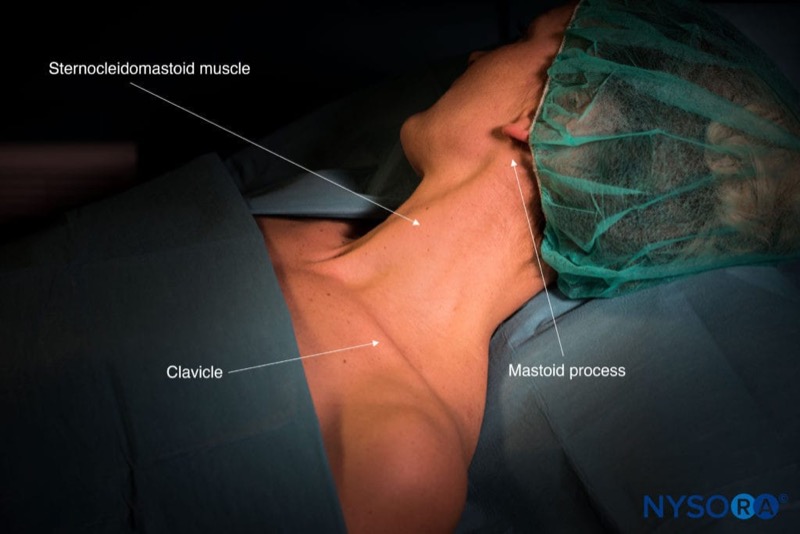
Fig-2. Functional innervation of the upper extremity muscles (myotomes).Patient position: Supine with a semi-sitting position and the head facing away from the side to be blocked.
External landmarks: Clavicle, sternocleidomastoid muscle, and external jugular vein (EJV), when visible.
Transducer position

Scanning
Different scanning techniques can be used:
A. Identify the carotid artery deep to the sternocleidomastoid muscle, and move the transducer posteriorly to visualize the anterior and middle scalene muscles. The brachial plexus is typically visualized at a depth of 1–3 cm.
B. Traceback technique:

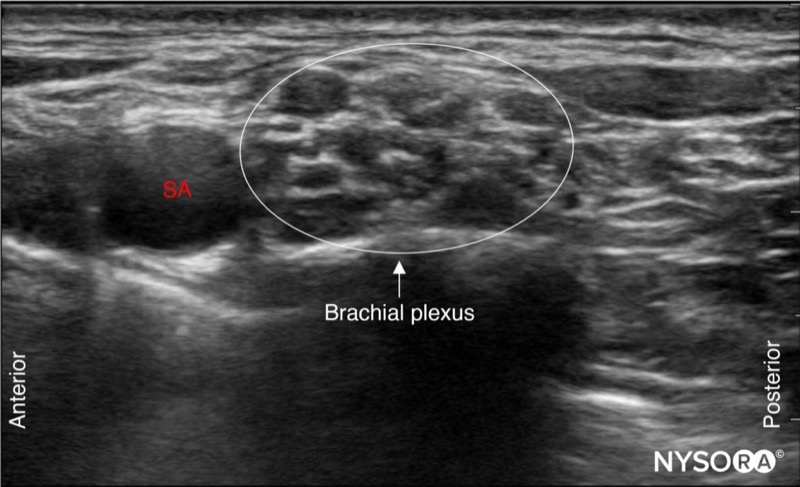
Depending on the depth of the field selected and the level at which scanning is performed, the first rib and/or the apex of the lung may be seen.
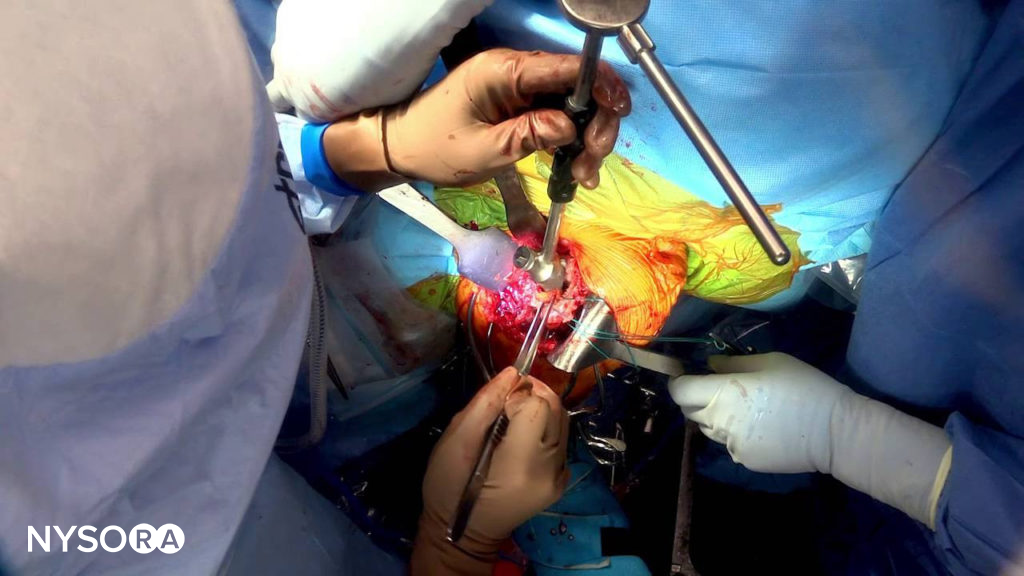
Needle insertion

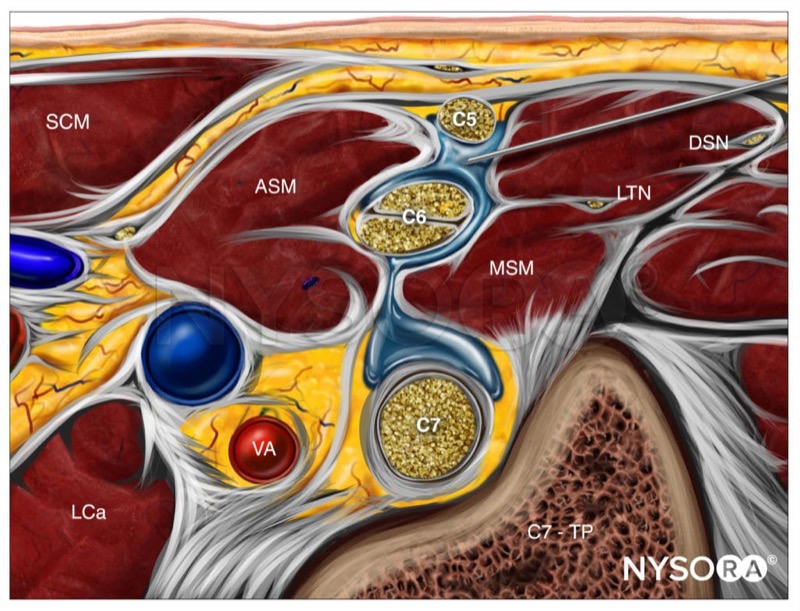
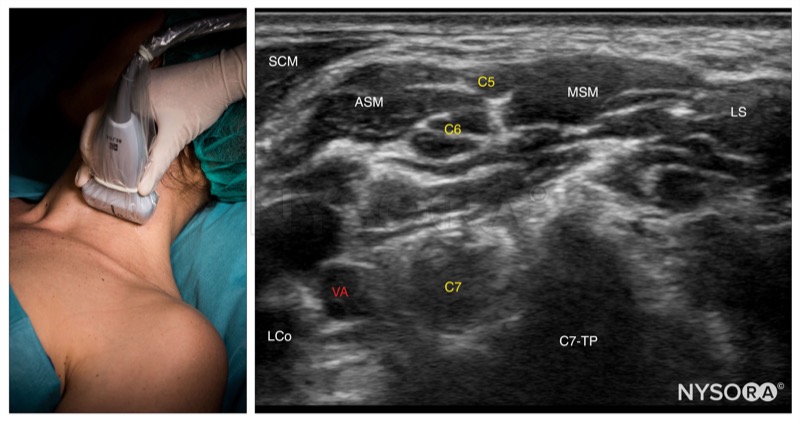

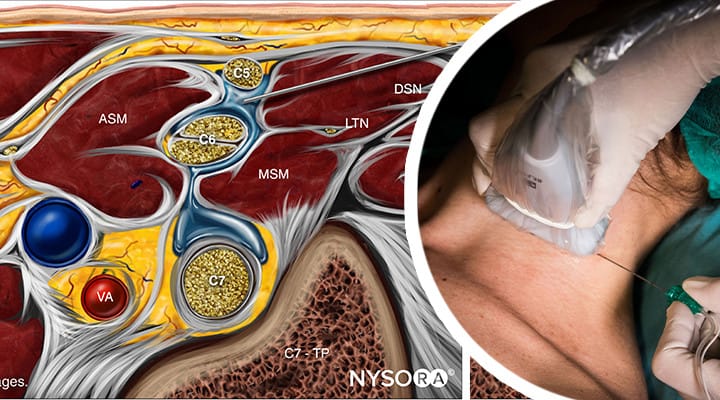
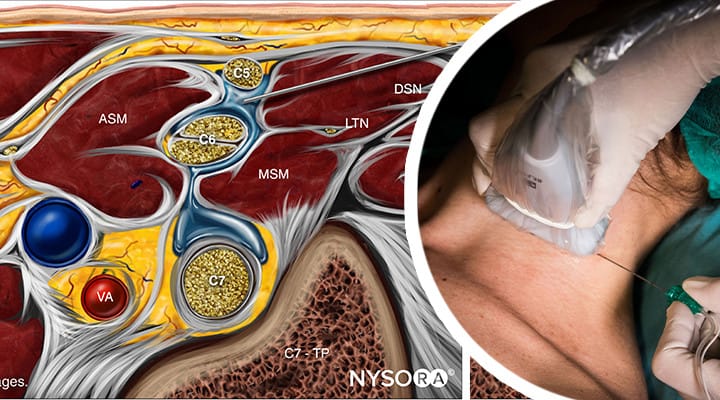
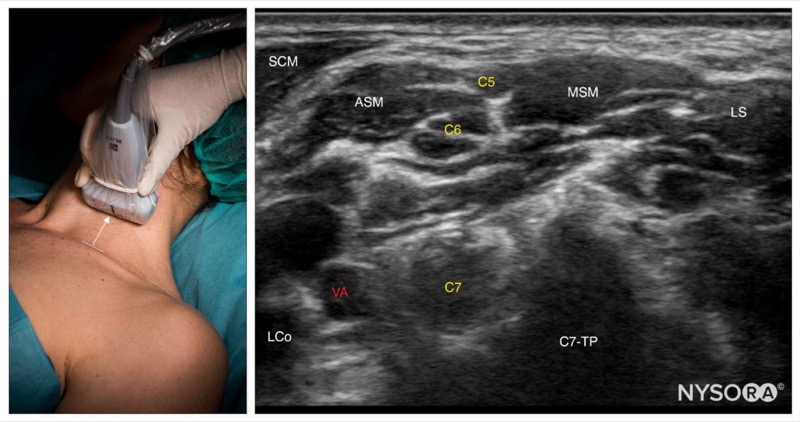
 Interscalene block; Reverse Ultrasound Anatomy with needle insertion in-plane. SCM, sternocleidomastoid; ASM, anterior scalene muscle; LCa, longus capitis muscle; VA, vertebral artery; MSM, middle scalene muscle; LTN, long thoracic nerve; DSN, dorsal scapular nerve; C7-TP, transverse process of C7.
Interscalene block; Reverse Ultrasound Anatomy with needle insertion in-plane. SCM, sternocleidomastoid; ASM, anterior scalene muscle; LCa, longus capitis muscle; VA, vertebral artery; MSM, middle scalene muscle; LTN, long thoracic nerve; DSN, dorsal scapular nerve; C7-TP, transverse process of C7.
Interscalene catheter

Important: Avoid LONG-acting local anesthetics in patients who cannot tolerate a decrease in lung function by 20% (phrenic nerve paralysis).