Analgesia for hip fractures and hip surgery.
Indications: Analgesia for hip fractures and hip surgery

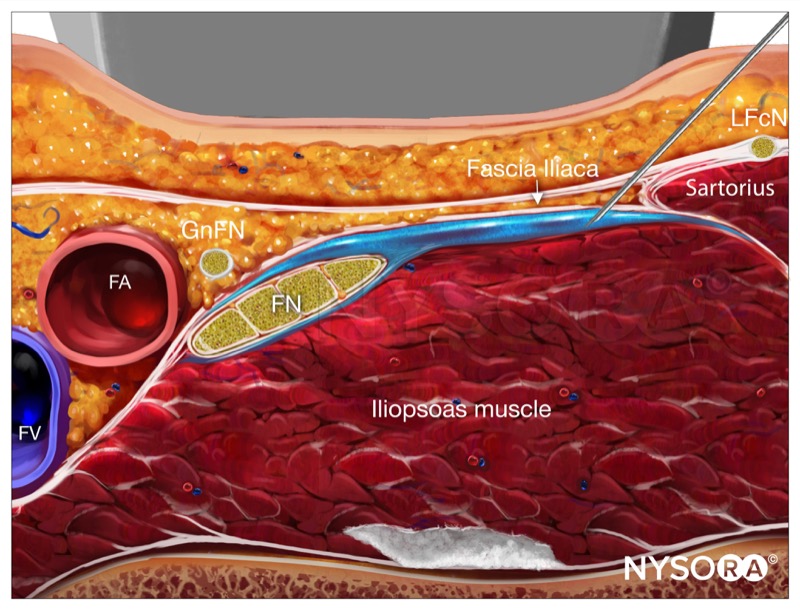
Goal: Local anesthetic spread underneath the fascia iliaca toward the lumbar plexus
Transducer: Linear
Needle: 22G, 5 cm short bevel
Local anesthetic volume: 20-40 mL
Functional anatomy
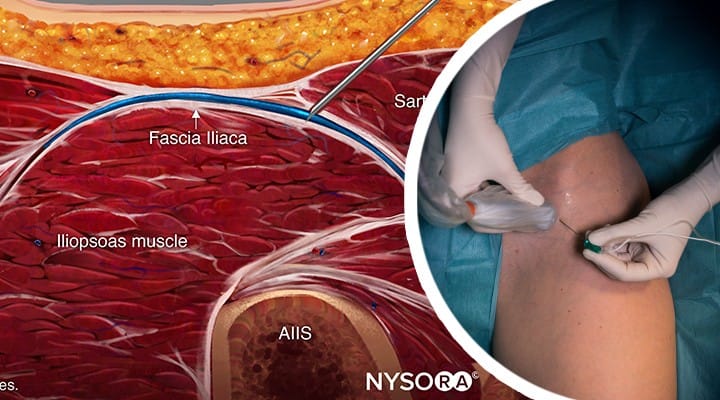
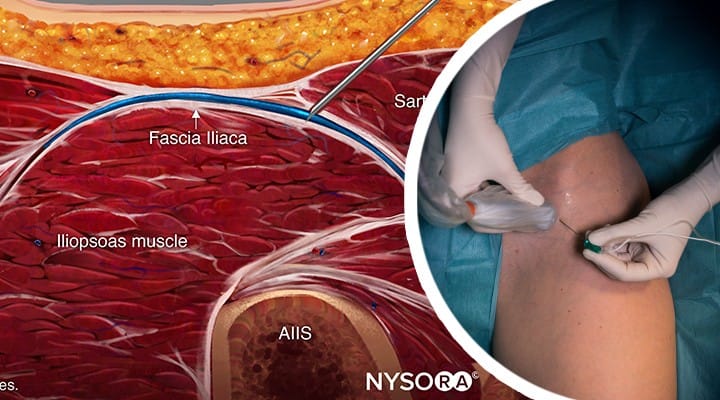
The fascia iliaca is located anterior to the iliacus muscle (on its surface) within the pelvis.
The femoral and lateral femoral cutaneous nerves lie under it.
Block rationale: A sufficient volume of local anesthetic deposited beneath the fascia iliaca, even if placed some distance from the nerves, has the potential to spread underneath the fascia and reach these nerves.
Potential spread underneath fascia iliaca toward the lumbosacral plexus has not been consistently demonstrated. Since the spread cannot be entirely controlled, this technique is primarily used for analgesia, not anesthesia.

Sensory and motor block occurs in the distribution of the nerves reached by the local anesthetic after injection underneath the fascia iliaca:


Patient position: Supine to facilitate access to the inguinal area.
External landmarks: Inguinal crease and the anterior superior iliac spine (ASIS).

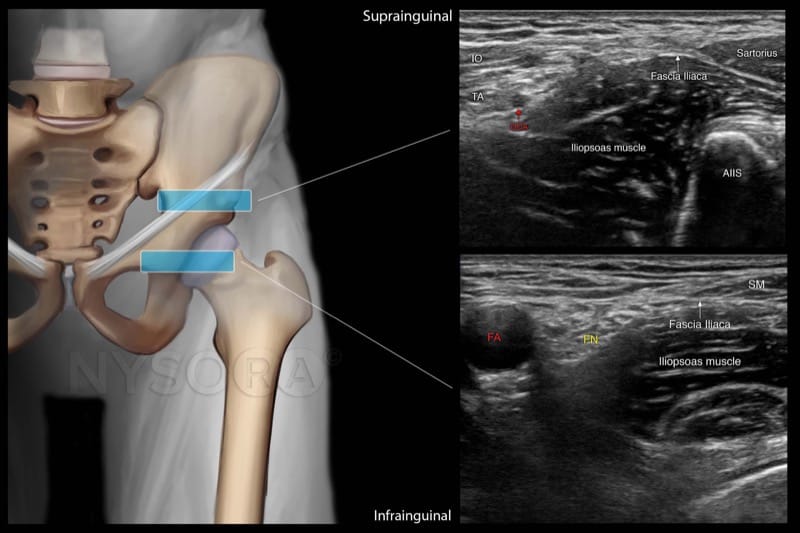
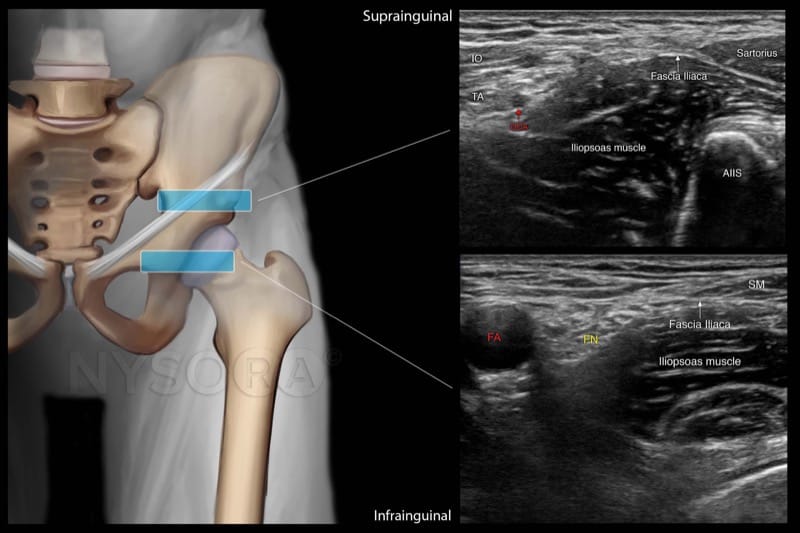
A fascia iliaca block using ultrasound can be performed either inferior or superior to the inguinal ligament.
Transducer position
Place the transducer in a transverse orientation at the femoral crease.

 Scanning
Scanning
1. Identify the femoral artery, vein, femoral nerve, the iliopsoas muscle, and fascia iliaca which covers the nerve and the iliacus muscle.


2. From this point, scan slightly laterally to identify the injection point away from the femoral nerve underneath the fascia iliaca.


Needle insertion
1. Insert the needle in-plane from a lateral to medial direction.


2. Place the needle tip underneath the fascia iliaca, away from the femoral nerve.
3. Inject 1-2 mL to confirm proper needle placement and complete the block with 20-30 mL of local anesthetic.

.jpg)
.jpg)
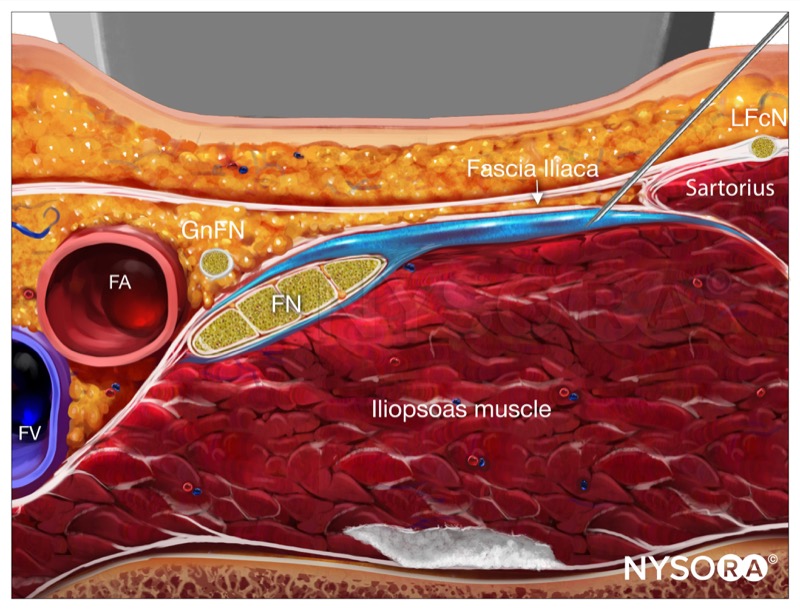
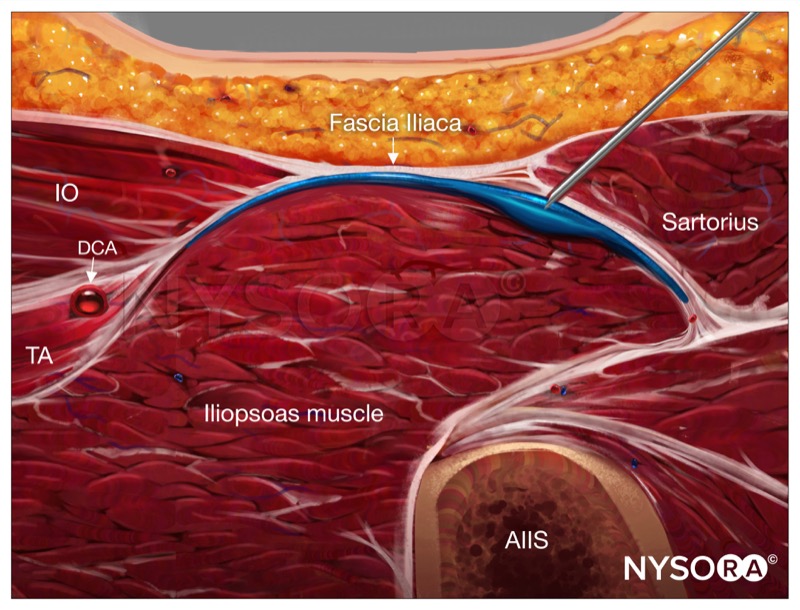
There are two possible scanning techniques for a suprainguinal approach:
1. Place the transducer in a sagittal oblique orientation medially to the anterior superior iliac spine, perpendicular to the inguinal ligament.


2. Slide the transducer medially, always perpendicular to the inguinal ligament, until the anterior inferior iliac spine is visualized.
3. Identify the sartorius and internal oblique muscles facing each other next to the inguinal ligament, creating a “bow-tie” or “hourglass” image. The deep circumflex iliac artery is frequently seen in between the transversus abdominis and the iliacus muscle, giving another confirmation of the layers.


1. Place the transducer in a transverse orientation over the femoral crease and identify the femoral vessels, femoral nerve, and fascia iliaca covering the iliacus muscle.

2. Slide the transducer laterally until the sartorius muscle is identified and from there slide the transducer cephalad until the anterior inferior iliac spine is visualized.

A systematic scanning starting from the femoral crease will help you identify the correct plane for injection for a suprainguinal fascia iliaca block. If you cannot find the correct image, go back to start from step #1.


Needle insertion
1. Insert the needle in-plane, from a lateral to a medial direction through the sartorius muscle and fascia iliaca.

2. After negative aspiration, inject 1–2 mL of local anesthetic to confirm proper injection plane between the fascia and iliopsoas muscle.

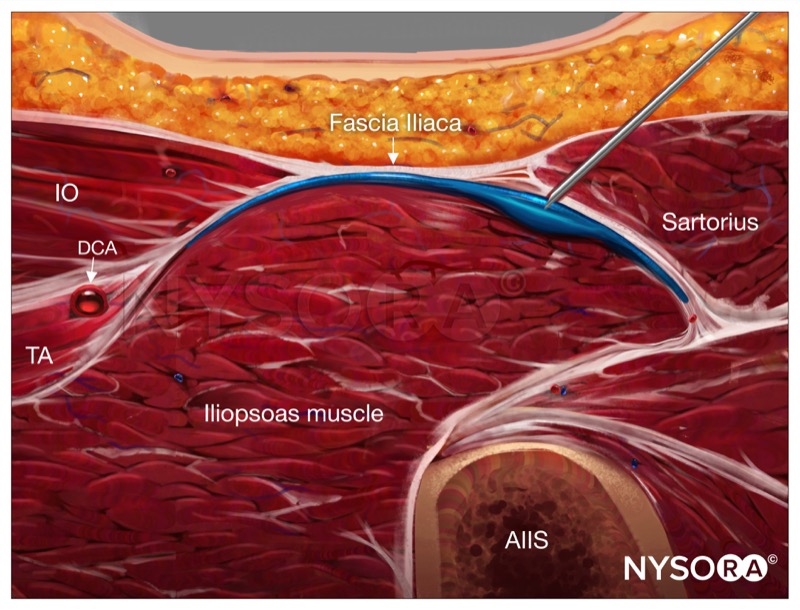
A successful injection will separate the fascia iliaca from the iliacus muscle by the local anesthetic.


.jpg)
.jpg)
Since this block depends on the distribution of a high volume of local anesthetic (20-40 mL) underneath the fascia, diluted concentrations of long-lasting local anesthetics are most commonly used (bupivacaine 0.25%, levobupivacaine, and ropivacaine at concentrations of 0.2%-0.3%). Higher concentrations may result in a prolonged motor block, numbness, delayed ambulation, and risk of local anesthetic systemic toxicity.
Common procedures: Total hip replacement, hip fractures, or hip revision.
